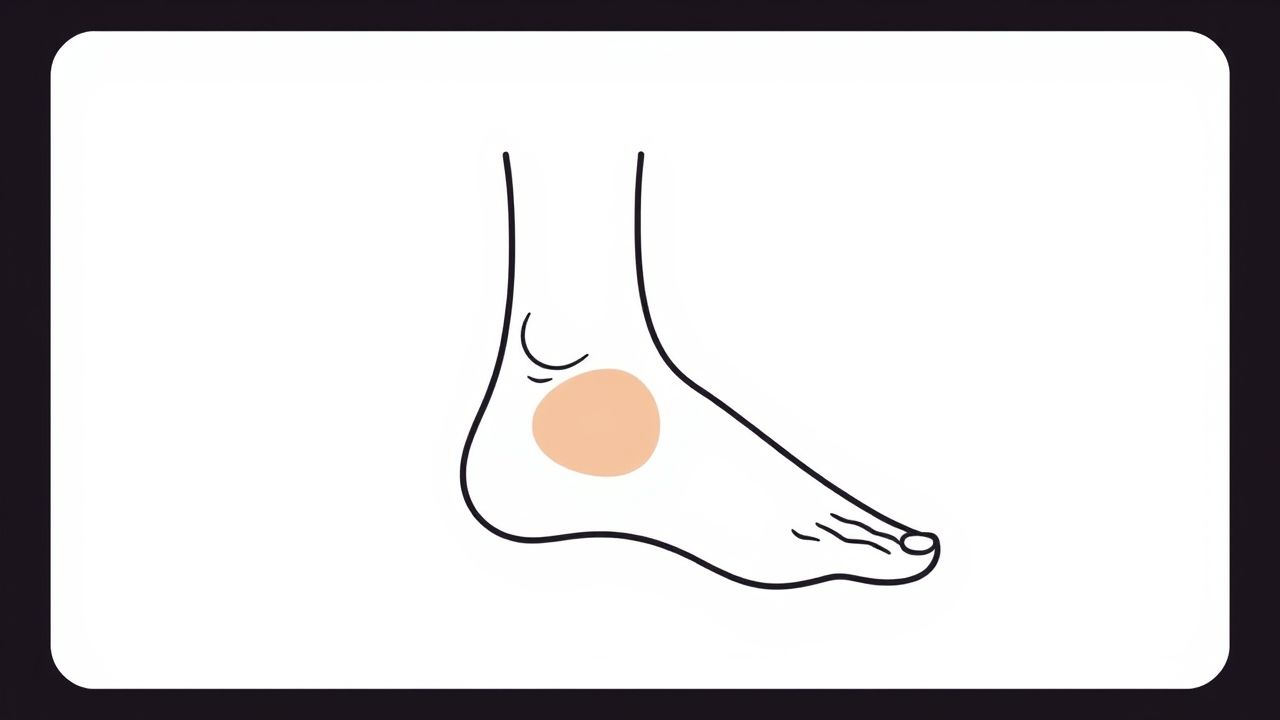
Callosity over the lateral malleolus is a common condition characterized by the formation of thickened, hardened skin in the area surrounding the outer ankle bone. This callus develops as a result of repetitive friction, pressure, or irritation on the skin surface, often caused by footwear, gait abnormalities, or other mechanical factors. While it might seem like a minor cosmetic or comfort issue, callosity in this region can lead to discomfort, pain, and even complications if left untreated. Understanding the causes, symptoms, treatment options, and prevention strategies is essential for effective management and maintaining foot health.
What is a Callosity?
A callosity, or callus, is a localized thickening of the skin that forms due to repeated mechanical stress. It is the body’s protective response to pressure and friction, where the skin produces extra layers of keratin to shield underlying tissues. Callosities are generally painless but can become uncomfortable or painful if they grow too thick or crack. Over the lateral malleolus, these callosities often form because of specific mechanical forces acting on this bony prominence.
Location and Anatomy
The lateral malleolus is the bony prominence on the outer side of the ankle, part of the fibula bone. It serves as an attachment point for ligaments that stabilize the ankle joint. Because it protrudes, this area is susceptible to rubbing against shoes or other surfaces, especially during walking or other repetitive motions. The skin here is relatively thin and less cushioned, which contributes to the risk of callus formation.
Causes of Callosity Over Lateral Malleolus
Several factors contribute to the development of callosities in this specific area
- FootwearIll-fitting shoes that are too tight or have rigid edges can rub against the lateral malleolus, causing friction and pressure.
- Gait abnormalitiesAbnormal walking patterns, such as overpronation or supination, can increase pressure on the lateral ankle, leading to skin thickening.
- Bone deformities or prominenceSome individuals have more pronounced lateral malleoli or structural foot deformities that predispose them to callus formation.
- ActivitiesRepetitive movements or activities that put stress on the ankle, like running, hiking, or standing for long periods, can contribute.
- Use of orthopedic devicesBraces or casts that apply pressure on the lateral malleolus may cause callosities.
Symptoms and Signs
Callosity over the lateral malleolus often begins as a small, rough patch of skin that gradually thickens. Common symptoms include
- Thickened, yellowish or grayish skin patch over the outer ankle bone
- Dry, rough texture with possible cracking or fissures
- Mild to moderate discomfort or tenderness, especially when wearing shoes
- In severe cases, pain during walking or standing
- Occasionally, inflammation or redness if the area becomes irritated or infected
Unlike corns, callosities are generally broader and less defined, though they can coexist. If the callosity becomes very thick, it may affect gait and increase the risk of skin breakdown or infection.
Diagnosis
Diagnosis of callosity over the lateral malleolus is primarily clinical, based on history and physical examination. A healthcare provider will examine the area, assess footwear and walking patterns, and rule out other conditions such as corns, warts, or skin infections.
In rare cases, imaging studies like X-rays may be ordered to evaluate underlying bony structures if deformities or fractures are suspected. This helps in understanding the mechanical causes and guiding treatment.
Treatment Options
Managing callosity over the lateral malleolus focuses on relieving pressure and reducing friction while promoting skin healing.
Conservative Management
- Footwear modificationWearing well-fitting shoes with soft padding around the ankle can reduce irritation. Avoiding tight or rigid shoes is crucial.
- Protective paddingUse of silicone pads, moleskin, or gel cushions around the lateral malleolus helps shield the skin from direct pressure.
- Regular moisturizingKeeping the skin hydrated prevents cracking and fissures, which can lead to pain or infection.
- Callus debridementGentle removal of thickened skin by a podiatrist using pumice stones or scalpel helps reduce discomfort and promote healing.
- Activity modificationLimiting activities that increase pressure on the ankle until symptoms improve.
Medical and Surgical Interventions
In cases where conservative measures fail, or when callosities cause significant pain or complications, further interventions may be necessary
- Orthotic devicesCustom orthotics can correct gait abnormalities that contribute to callus formation.
- Surgical correctionFor patients with bone deformities or prominent lateral malleoli causing recurrent callosities, surgery to reshape the bone may be considered.
- Treatment of secondary infectionsIf the callosity cracks and becomes infected, antibiotics or topical treatments may be required.
Prevention Strategies
Preventing callosity over the lateral malleolus revolves around minimizing friction and pressure on the skin in this area.
- Choosing appropriate footwear with enough room and cushioning around the ankle
- Using protective pads or sleeves to shield vulnerable skin
- Maintaining good foot hygiene and regular moisturizing
- Addressing gait abnormalities with professional assessment and orthotics
- Avoiding prolonged standing or activities that exacerbate pressure on the ankle
When to See a Doctor
While callosities are often benign, medical attention is advisable if
- There is persistent pain or discomfort despite home care
- The callosity cracks, bleeds, or shows signs of infection such as redness, swelling, or pus
- Difficulty walking or using footwear due to the callosity
- Underlying conditions such as diabetes or peripheral vascular disease, which increase the risk of complications
Callosity over the lateral malleolus is a common skin condition resulting from repeated friction and pressure at the outer ankle. Though often mild, it can cause discomfort and lead to complications if untreated. Proper diagnosis, footwear modification, protective measures, and appropriate treatment help manage symptoms effectively. Prevention through good foot care and addressing mechanical causes is key to avoiding recurrence. For individuals experiencing pain or complications, consulting a healthcare professional ensures timely intervention and optimal outcomes.